
Do you know this is a question I often get asked and I know when I worked in acute hospitals, I often got asked by doctors to help patients with their meds. When a cousin recently asked me, I struggled to find a lot of information online and then when a patient asked me, I got online to my feeding professional groups and asked them?
Below is a combination of my techniques and my colleague who I am so grateful for opening sharing their thoughts and own experiences.
Do you know I actually have difficulties swallowing tablets? It made the session planning for my patient very interesting because I started to realise that there were lots of people who struggled with this too.
First thing to think about: what is it about the tablet that makes it hard for you or your child to swallow? Is it:
- The taste of the dissolving tablet? Nothing more gag triggering for me that a Panadol home brand tablet. Something that is in the gel coating is much easier.
- The smell? For my patient, the smell was a big issue
- The size? For me and a colleague, the bigger the pill, the harder it was.
- The shape? A mother pointed this out to me something with rough or sharp edges (eg pill cut in half) gives more sensory input to trigger a gag.
- While colour doesn’t seem to be the bigger triggers, combined with a past experience, it could also trigger more anxiety in some people.
Where is it getting stuck? We have all had the experience of swallowing food and it “feels stuck” – I imagine that it is just moving slowly down our oesophagus and often might have not chewed enough, swallowed too big or to dry. With consecutive swallows of water, it often clears but it doesn’t feel nice when it happens right? Combined with lots of frequent exposures to this happening or a history of reflux and exacerbated and sore throats, this can feel very painful.
So having a conversation about what triggers the “worry” for that child is important. Depending on their age, you can also talk about the airway vs oesophagus (tube to your stomach) and build in detail as you need it. Mainly that when the airway is open, the stomach tube is closed and vice versa. So your epiglottis (a flap) actually closes your airway when you swallow. Simiarly when you swallow, you momentarily stop breathing – scary as that might sound, it’s only for a tiny second and it protects your airway so the food goes down the right way. This video is a very basic one but there are many similar and more detailed ones online.
So how do you teach a child to swallow tablets?
Step 1: Practice the technique of swallowing on its own.
There are several ways to practice this and this video goes through them in a step by step manner: https://youtu.be/MXFMZuNs-Fk

Here is a summary of my techniques:
- Try taking a small sip of water, move it to the back of your throat, hold your breath and then effortfully swallow
- Alternatively, take a sip of water, move to the back of your throat and then tip your head down so that your chin touches your chest then swallow. This chin tuck is a common speech pathology technique to help your airway close
- Some people find the opposite works better – ie, take a sip of water, move it to the back of your throat and then tip your chin up (looking at the ceiling) and then swallow. I actually find that this makes the muscles in my throat work harder but a lot of patients find this easier.
- In the video by Alberta Children’s Hospital Foundation, they suggested a head turn to the side to create an effortful swallow
- My colleague Holly Tickner from Taste Buds Speech Pathology has a very clever up and back technique where she teaches her patients to take a sip of water, touch the tip of their tongue to their alveolar ridge or just behind the ridge (the bump behind your front teeth) and then move the water back while the back of your tongue drops down to swallow
- When I swallow, I actually do a double swallow – ie, take a big mouthful of water and the tablet in my mouth, swallow a bit of water, then use my tongue tip to move the tablet back and swallow the second time. 2 swallows seems less likely to trigger a gag for me.
Why not practice all 6 techniques with your child and see what helps them the most. Watching you tube videos of ducks and frogs swallowing will also help a child motor plan the aspects of swallowing so they can step by step help it happen cognitively.

Step 2: Think about the “chaser”
This brings in the sensory cues and I have my Occupational Therapist colleague Gillian Griffiths from Sensational Mealtimes to thank for her ideas. She reminded me about the sensory properties of liquids and how they can trigger faster swallows for some people.
- Cold water vs room temperature (the coldness of the water may help)
- Carbonated drinks (eg lemonade, sparkling water) vs water (the bubbles may help)
- Melted ice cream/yoghurt/fruit puree vs water (the thickness may help)
I definitely find it easier to swallow with sparkling water and the colder the better – it triggers a faster swallow. What works for your child?

Step 3: Grade up in size
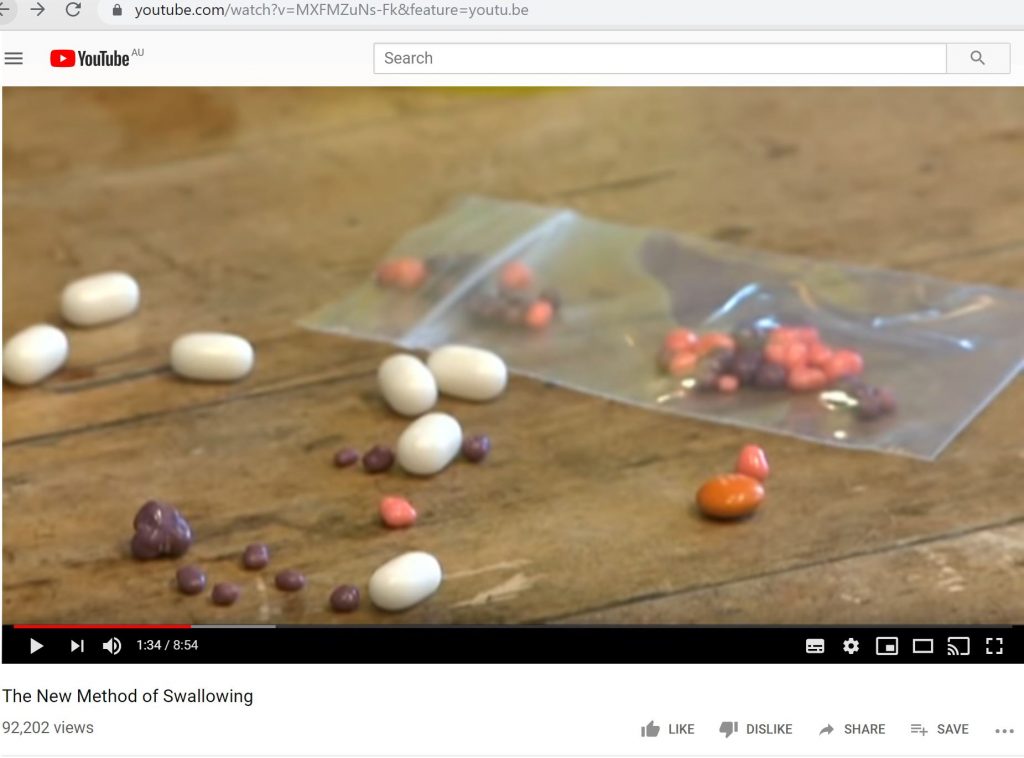
All of my colleagues recommended thinking about the size of the tablet and grading up in difficulty from small (and melts) to bigger….
- Ice chips – build up on size
- Sprinkles
- Tic tacs
- Shavings of meltable lollies or foods (eg banana lollies, musk sticks, rice bubbles)
- Mini MnMs – cut in ¼ then ½ then whole
- Smarties
- Lolly snakes cut up in different sizes (the softer texture helps go down easier)
- Vitamin C tablets cut in ½ then whole
- Bigger multivitamin tablets
You can also buy empty dissolvable capsules of different sizes where you can chop the tablets into and fill (if your chemist says this is okay to do of course). This will exclude the smell and taste aspect of chalky tablets.
Of course, you can always crush tablets (if your chemist says this is fine to do) and mix with jam, honey or yoghurt spoonfuls. Other professionals suggested chewing on a cracker and then before swallowing, giving the child the tablet with the chewed cracker mouthful to swallow. All excellent technique but the point of this blog post was to actually teach your child to swallow it whole.
My clever colleague Jennifer Morris Meyers from America suggested this “GMS pill takers cup”– the idea is that you place the tablet in the holding area of the cup and then “take a drink” and it floats the pill in the liquid for you. I imagine you will need to take several swallows all in one go to make this cup work well.
Step 4: think about the time of day
For some people the time of day can really make a difference – I know when I wake in the morning and need to take a pill, I am more likely to gag. For some people, particularly those with muscle tone fatigue, swallowing pills at night can trigger more gag and difficulty. If your tablets are time specific, chat with your doctor about the window of time and see if eating a meal then taking a tablet or taking the tablet before makes a difference.
Step 5: lastly – practice and persistence: don’t give up!
Swallowing tablets takes time and knowing that is very important in itself. It won’t happen immediately – it takes time for your sensory and motor system to feel confident in knowing what to do and what works best. But don’t give up either just because you gagged once. Try swallow practice every day, grade up in size and play around with the technique of swallowing (step 1) and “chaser” (liquid or puree). With time and practice, most of the people I work with manage to get it. And for me, it’s the belief – even if I need to take a tablet and I gag the first time, I remind myself that I can do it and give it another go (or several goes and drinks of water). Power of the mind really!

Wishing you happy mealtimes (and easier swallowing tablet moments!)
Val
Paediatric Feeding Speech Pathologist @ Let’s Eat! Paediatric Speech Pathology

This website and information on this blog post is provided for educational purposes. It is not meant or intended to replace Speech Pathology assessment and management nor medical or nutritional care for a child. It is recommended that you discuss any concerns or questions you might have with your Speech Pathologist and managing Doctor and develop an individualised team plan specifically for your child.

